Implantology counts on tools that are capable of extraordinary esthetic results. In the past, implantology as a science had demonstrated the capacity for the methodic reproduction of osteointegration. However, under the light of contemporary knowledge, there is a search for the predictability of the peri-implant tissue marginal stability (absence of recesses and presence of papilla), decreased morbidity and treatment times. Never before has implantology experimented the magnitude of the present search for the harmony in the level, contour, color, texture, quantity and quality of peri-implant mucosa.
The longevity of peri-implant pink esthetics is possible and predictable However, the interpretation leads to the idea of immutability, with what is not to be altered, must be used with precaution. After all, the feasibility of the immutability of peri-implant tissues through time is arguable. Nevertheless, their longevity has been tested in innumerable researches, and, presently, we know that the long-lasting marginal stability is influenced by several factors such as:
• Minimally traumatic exodontia;
• Therapeutic approaches (immediate implant, filling of the alveolus with low reabsorption rate biomaterials and guided bone regeneration) which minimize post-exodontia bone loss.
• Type of implant/prosthetic component connection;
• Tissue phenotype;
• Tridimensional positioning of the implant.
The knowledge of those determining factors allows for preventive and interventionist approaches for esthetic longevity. The level of the bone crest influences the positioning of the peri-implant mucosa margin and the presence of the papilla relates to the integrity of the interproximal bone septum.
Minimally traumatic exodontia
Minimally traumatic exodontia, flapless and without pendulum movements is the primordial phase of the marginal stability of the peri-implant tissues, since it minimizes the magnitude of the inevitable bone loss after exodontia. That happens, quick and intensely, horizontally (more accentuated) and vertically. In this repairing dynamics, the reabsorption of the fasciculate bone (alveolar cortical portion that receives the Sharpey fibers of the periodontal ligament) is relevant. The fasciculate bone is tooth-dependent and after exodontia, it will be integrally reabsorbed because it will lose its function (to promote the insertion of the Sharpey fibers of the periodontal ligament) and the main source of vascularization (through the Volkamann canals of the periodontal ligament). The pertinence of the loss of the fasciculate bone is related to the high prevalence of thin vestibular walls (practically constituted by that tooth-dependent tissue). This way, the vestibular bone loss is accentuated with unquestionable aesthetic repercussions. According to this idea, the concepts of alveolar conservation or reconstruction after exodontia are erroneous, the alveolus exists because of the presence of the tooth.
Approaches that minimize the volume of bone loss after exodontia
After exodontia, there are three possible therapeutic alternatives: filling of the alveolus with blood clot, filling of the alveolus with low-reabsorption rate biomaterial and/or guided bone regeneration or immediate implant. Unfortunately, the most popular technique is the filling of the alveolus with the blood clot, and it is also the least recommended. Odontology based in scientific evidences (systematic reviews and randomized prospect studies) demonstrate a greater magnitude of bone loss with the filling of the alveolus with the blood clot, in comparison with the approaches that had the purpose of minimizing bone reabsorption (filling with biomaterial with low reabsorption rates with or without guided bone regeneration or immediate implant).
In a hierarchical scale, the first option should be the immediate implant. If that is not possible, the choice will be for the filling of the alveolus with biomaterial with or without guided bone regeneration. The immediate implant allows for the maintenance of the parabolic shape of the peri-implant mucosa margin, similar to the adjacent teeth (with the gingival margins parallel to the cement-enamel junctions). The palatine approach promotes the presence of the gap between the implant and the vestibular wall. That gap must be filled with biomaterial with low absorption rates (preferably a biphasic ceramic), to compensate for the inevitable reabsorption of the fasciculate bone. Presently, the immediate implant can be recommended even with the previous absorption of the vestibular wall, if there is proximal integrity. The immediate implant, with the concurrent reconstruction of the vestibular wall is a routine and predictable approach.
Type of implant/prosthetic component connection
The integrity of the bone crest is dependent of the type of implant/prosthetic component connection. In the hexagonal, there will be inevitable horizontal and vertical bone losses, with the configuration of bone “saucerization”. That peri-implant bone loss derives from the micromovement of the implant/prosthetic component connection, presence of the gap and from the biological space positioning. Consequently, the micromovements will promote the apical migration of the junctional epithelium; the gap will be populated by bacterial biofilm and the biological space will form below the prosthetic component/implant interface. Remember that in the hexagonal connections, the implants are placed on level or slightly below the bone crest. In this development, the junctional epithelium will not adapt (through the basal and hemidesmosome lamina), on the interface (placed on level or slightly apical to the bone crest) with micromovements and contaminated by the bacterial biofilm. Soon, there will be vertical bone loss of approximately 1.5 to 2.0mm (necessary space for the adaptation of the junctional epithelium and conjunctive adhesion) and the biological space will form on the implant. Adding to that, in hexagonal connections, there are horizontal bone losses of 1.3 to 1.4mm.
In conic connections, there will be no micromovements, there will be no gap/biofilm and the biological space will be formed coronal to the prosthetic component/implant interface. Remember that in the conic connections, the implants are positioned 2.0mm apical to the bone crests. In that process, the junctional epithelium and the conjunctive adhesion will form on the prosthetic component. The peri-implant physiologic bone loss is rare, there is evidence of marginal stability of the peri-implant tissues.
From what was exposed, are the hexagonal connections contraindicated for aesthetic areas?
The answer is: no, they are not. However, the professional that knows the irrevocable vertical and horizontal bone losses should analyze the tissue phenotype and be careful with the tridimensional positioning of the implant. Thinner phenotypes (thin or intermediate) associated to peri-implant bone losses will result in marginal instability. Add to that the preoccupation with the tridimensional positioning, in function of horizontal bone losses for the integrity of the proximal papillae. Therefore, the hexagonal connections are not contraindicated in places with an aesthetic demand, but, in situations as such, the priority choice should be for conic connections.
Tissue phenotype
The tissue phenotype (thickness) is intrinsically related to the marginal stability of periodontal and peri-implant tissues. The tissue thickness of the peri-implant gingiva/mucosa and of the vestibular wall are evaluated. Logically, the tissue phenotype is more critical for hexagonal connections. Non-thick phenotypes are a synonym of marginal instability and, suggestive of phenotypical alteration indication. Unfortunately, the prevalence of non-thick phenotypes is very high.
The phenotypical alteration of the peri-implant mucosa is carried out by means of grafts with subepithelial conjunctive tissue or pediculate techniques (i.e.: the “roll” technique). The phenotypical modification of the vestibular wall is usually achieved with the use of biphasic ceramics associated to guided bone regeneration.
Tridimensional positioning of the implant
The tridimensional positioning based on a reverse plan is crucial for the absence of recession (level of the vestibular bone crest) and for the presence of the papilla (level and existence of the interproximal septum). In that context, the horizontal bone loss (mesial, distal, vestibular, lingual/palatal) of 1.3 to 1.4mm correlated to the hexagonal connections translates into an important factor for the correct positioning of the implant(s).
The minimum distance between an implant with a hexagonal connection and an adjacent tooth, for the existence of the interproximal bone septum is 3.0mm. In the vestibule/lingual direction, the positioning of the implant must guarantee the existence of the vestibular wall. However, in the case of conic connections or switching platforms, due to the absence of horizontal losses, the implants may be located closer to the other teeth or closer to one another.
The possibility for the customization of the prosthetic component (between 0 and 20°), allowed by the Arcsys system, is a powerful and exclusive tool that facilitates the surgical/prosthetic planning. However, the customization does not eliminate the necessity of the reverse plan.
Clinical Case
Clinical case courtesy of professors Bernardo Passoni and Rodrigo M. Ferreira.
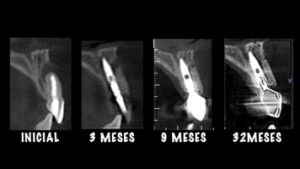
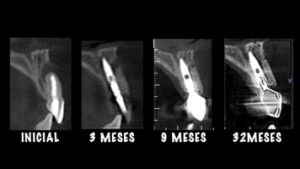
The clinical case that illustrates this article synthetizes the preventive and therapeutic approaches. Therefore, the procedures carried out were: minimally traumatic exodontia; placement of an immediate implant with frictional connection and palatal approach; filling of the gap with biphasic ceramics; subepithelial tissue grafting and manufacture of prothesis over teeth and over implant.














Author: Ricardo de Souza Magini
Head Professor Universidade Federal de Santa Catarina (UFSC).
Professor of the Graduate Program in Odontology at UFSC, Implantology area.
Specialist, MSc and Doctor in Periodontia from Universidade de São Paulo – Dental College of Bauru.